Cholera epidemics in Victorian London
 During the 19th century, four major outbreaks of cholera between 1832 and 1866 ravaged
London communities and led to the death of tens of thousands of people.
During the 19th century, four major outbreaks of cholera between 1832 and 1866 ravaged
London communities and led to the death of tens of thousands of people.
Cholera ('Asiatic cholera') had spread from the Indian subcontinent to Europe. Attempts were made to stem the arrival of the disease, with the quarantine of incoming ships (Gazette issue 18807). Coastal residents were warned of ‘the danger to which they expose themselves by engaging in illicit intercourse with persons coming from the Continent; and should appeal to their fears in warning them of the imminent risk which they incur by holding any communication with smugglers, and others who may evade the quarantine regulations.’ (Gazette issue 18863)
Once contracted, symptoms of this deadly disease included stomach cramps, ‘looseness of the bowels’ (Gazette issue 18863), vomiting, severe pain in the limbs and severe dehydration that, if left untreated, ‘may suddenly assume a fatal form’ (Gazette issue 20903), sometimes within hours of the first symptoms.
Sufferers appeared ‘sharp and contracted, the eye sinks, the look is expressive of terror and wildness…. The skin is deadly cold and often damp, the tongue always moist, often white and loaded, but flabby and chilled like a piece of dead flesh’ (Gazette issue 18863). There was no known cure, and the sense of panic among the populace – and government – was palpable.
The first identified and reported case of cholera in Britain was in October 1831, when keelman William Sproat of Sunderland contracted the disease and died just three days later. So why did it spread so rapidly once it reached the capital in 1832?
London’s rapid growth had not been matched by the developments needed to deal with the huge amount of sewage that was being produced. Sewage was coming in to contact with drinking water and contaminating it. And as many people used river water as their source of drinking water, the disease spread with ease.
Miasma theory: the deadly stench?
The accepted theory at the time was that cholera was air-borne, transmitted via poisonous vapours, ‘miasma’, from rotting of organic matter. It seemed to be backed up by the many falling victim to the disease living in overcrowded slums where the air was most polluted.
In actual fact, cholera is a water-borne disease produced by the bacterium vibrio cholera and transmitted via contaminated water sources. In the mid-1800s, London’s poorest were surrounded by their own and others’ filth, as basement cesspits overflowed due to the lack of efficient sewage system. The Thames, the main source of drinking water for residents, became more and more polluted.
Edwin Chadwick and public health policy
In 1831, The London Gazette published a Board of Health report that attributed cholera to, ‘the poor, ill-fed, and unhealthy part of the population, and especially those who have been addicted to the drinking of spirituous liquors, and indulgence in irregular habits’ (Gazette issue 18863). The rather paternalistic tone implied that to some degree the poor brought it on themselves, rather than it being a result of the appalling conditions they were reduced to living in.
Rapid population growth, overcrowded housing and sanitation problems needed to be addressed. Edwin Chadwick, public health campaigner, was tasked with tackling public sanitation. Though he believed toxic miasma to be the means of its transmission, he went against the dominant view of urban poverty being a result of laziness or immorality, but rather due to the conditions in which people lived.
In February 1832, the Cholera Morbus Prevention Act (London Gazette 18909) became law and allowed some powers to local Boards of Health, but it had little impact on the epidemic of 1832.
In 1848, the Nuisances Removal and Diseases Prevention Act (Gazette issue 20637) – the ‘cholera bill' – was passed to help stop the spread of cholera during the 1848-9 epidemic. Property owners were encouraged to clean their dwellings, to prevent ‘atmospheric impurity’, and ‘Householders of all classes should be warned, that their first means of safety lies in the removal of dung heaps and solid and liquid filth of every description from beneath or about their houses and premises’ (Gazette issue 20903). The establishment in 1848 of the Metropolitan Commission of Sewers (Gazette issue 20895) was to bring its sewer and drainage infrastructure under the control of a single public body. Properties were to be cleaned and connected to sewers.
However, as the suggested remedy was to effectively dump the contents of cesspools and raw sewage pits into The Thames, it only helped to exacerbate the problem. The middle classes also contributed, with the increasing popularity of the flushing water closet adding to the large amounts of sewage amounts reaching the river. The 1848-9 cholera epidemic killed over 14,000 victims.
The Metropolitan Board of Works was set up in 1855 after the Metropolis Management Act was passed (Gazette issue 21764) to take control of the sewers with the aim that ‘the arrangements provided by that measure will lead to many improvements conducive to the convenience and health of this great city’.
London was not the only metropolitan area in cholera’s grip. For example, epidemics occurred in Liverpool in 1849, 1854 and 1866. The Sewerage and Drainage of Liverpool Act passed in 1846 allowed for a medical officer of health to be appointed to inspect and report on the sanitary state of the area and to point out ‘nuisances’ that might contribute to disease (Gazette issue 20671).
Dr John Snow and the Broad Street cholera outbreak
Despite miasma theory remaining widespread, the doctor and anaesthetist John Snow’s investigation suggested another means of transmission more likely. Snow’s conclusion by 1849, in his paper, 'On the Mode of Communication of Cholera', was that cholera spread through ingesting contaminated water, rather than inhaling a noxious form of bad air.
The Soho district of London was particularly overcrowded and unsanitary. Snow had identified the source of the cholera outbreak in this area, which had killed more than 500 people in 10 days, as the Broad Street pump. He had convinced the authority to disable the pump by removing its handle.
Snow had sought evidence to back up his theory, such as a workhouse that was close to the Broad Street pump and a prime site for cholera to take hold. But only 5 of the 530 inmates had contracted cholera, because nobody from the workhouse drank the pump water, as the building had its own well. And at the Lion Brewery, workers were given an allowance of free beer every day so never drank water, and there were no fatalities.
The 'Great Stink'
Despite the evidence that Dr John Snow presented to the medical establishment (Snow died in June 1858), public health officials were reluctant to ascribe to his theory. Nevertheless, the need to clean up the polluted Thames once and for all was irrefutable.
When the Great Stink during the hot summer of 1858 drove MPs out of Parliament due to the stench emanating from the river, a more determined attempt was made to clean up The Thames, with vocal support for a reform of policy.
On 15 June 1858, Disraeli tabled the Metropolis Local Management Amendment Bill. Within a record 18 days, a bill was created, passed, and signed into law that would refurbish the entirety of the River Thames, ‘for the improvement of the main drainage of the metropolis, and for preventing, as far as may be practicable, the sewage of the metropolis from passing into the river Thames within the metropolis’ (Gazette issue 22391).
The engineer Joseph Bazalgette (Gazette issue 24095) developed a systematic plan for the city's sewers. As chief engineer on London’s Metropolitan Board of Works, Bazalgette was primarily responsible for the creation of an extensive network of sewers under the streets of central London that diverted waste to the Thames Estuary. The project was completed in 1875.
The last British cholera epidemic was in 1866 (Gazette issue 23199).
Further reading and sources
Barnett, R, 2013, John Snow and cholera [accessed 28/01/16]
Lemon, J, nd, Cholera in Westminster [accessed 28/01/16]
Snow, S, Commentary: Sutherland, Snow and water: the transmission of cholera in the nineteenth century, International Journal of Epidemiology, Oxford Journals [accessed 28/01/16]
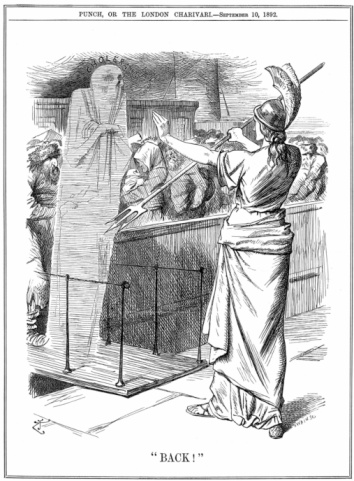
Image: Britannia holding back Cholera at British ports
Publication date: 1 February 2016
